|
Reference List
- Garry
R. Laparoscopic excision of endometriosis: the treatment of choice?
British Journal of Obstetrics & Gynaecology 1997;104:513-15.
- Redwine
DB. Conservative laparoscopic excision of endometriosis by sharp
dissection: life table analysis of reoperation and persistent or
recurrent disease. Fertility & Sterility 1991;56:628-34.
- Marcoux
S, Maheux R, Berube S. Laparoscopic surgery in infertile women with
minimal or mild endometriosis. Canadian Collaborative Group on
Endometriosis. N Engl J Med 1997;337:217-22.
- Cooper, Reid reference?
Back to top of page
______________________________________________
How old is endometriosis?
Late 17th and 18th century European descriptions of the disease.
Knapp VJ. Fertility & Sterility 1999; 72:10-14
_______________________________________________
This
recent article comes from the History Department at the State
University of New York and notes that endometriosis was described in
European history at least 300 years ago. The author notes that despite
increasing recognition of the problem, even today the disease receives
inadequate press. By way of example the "Encyclopedia of Medical
History" published in 1985 fails to mention it nor do more recent
publications as late as 1997.
The first detailed description of wide ranging peritoneal endometriosis was put forward by Daniel Shroen in 1690.
Despite
the many symptoms, it is striking over the years that recurrent
practitioners recognised the wide ranging extent of the problem and the
capacity for endometriosis to have a significant effect on the general
well being of the affected individual. It has been described in 1776
"..in its worst stages, this disease affects the well-being of the
female patient totally and adversely, her whole spirit is broken, and
yet she lives in fear of still more symptoms such as further pain, the
loss of consciousness and convulsions."
The significant pain, resembling
labour, associated with the disease has long been noted and at its
worst was described by various 18th century investigators as
"overwhelming", "oppressive", "convulsive", "atrocious" and "tortuous".
Countering the thought that the
problem was simply "hysteria" (the derivation incidentally coming "from
the womb"), in 1776 it was asserted that "hysteria is not an
idiosyncrasy that we can attribute to the female portion of the
population, it is obviously a major symptom of this deeply rooted
disease." In 1797 another physician questioned who would not be nervous
and hysterical , "...what with the sad state and anguish of this
disease. Women are tortured by the pain associated with this disorder,
followed thereafter by a struggle with all of its other myriad
symptoms."
Reading through these descriptions,
and with the knowledge that perhaps 10 to 15% of the population have
endometriosis, it seems almost unbelievable that in the year 2000 the
disease still remains so poorly described and understood.
Back to top of page
_______________________________________________
Advanced and Recto-Vaginal Endometriosis
_______________________________________________
Dr G D Reid
University of New South Wales, Sydney, Australia
Endometriosis
is a disease which continues to be poorly treated. Drugs are still used
to treat advanced disease when there is absolutely no evidence for
their efficacy. Hysterectomy is still performed for a disease that by
definition is "extra-uterine". Myths and false concepts are carried
from one textbook to the next.
Endometriosis is considered to be a
modern disease, and does not rate a mention in any contemporary
textbook of medical history. It has even been suggested that
endometriosis is the result of industrialisation, yet Daniel Shroen1
described endometriosis in great and graphic detail in 1690. He
described it as a disease affecting the pelvic surfaces, the broad
ligament, the bladder and the bowel. He described its progressive
nature, and its tendency to form adhesions. He spoke about its
vascularity, or the recently rediscovered importance of angiogenesis.
He described endometriosis as a disease with onset at puberty, and
adolescent endometriosis is still denied as a real entity by many
modern gynaecologists. Finally he claimed no originality for his work
and spoke about endometriosis in the tone of a commonplace disease.
There has been much debate about the
aetiology of endometriosis in general, and specifically about deep
rectovaginal endometriosis. Sampson's theory (1927) of retrograde
menstruation and cell implantation continues to be regarded as the
basis for most peritoneal endometriosis and there is much
circumstantial evidence in support of this. In 1919, Meyer suggested
that coelomic metaplasia or transformation of pluri-potential
mesenchymal cells from one cell type to another might account for some
endometriosis. Indeed it is otherwise impossible to explain the
occasional reports of endometriosis occasioning in male subjects.
Halban (1925) suggested that lymphatic dissemination of endometrial
cells may occur, and Sampson (1927) once again acknowledged that
vascular dissemination probably accounts for occasional reports of
widely disseminated endometriosis. Iatrogenic transplantation to
surgical wounds in the abdominal wall has also been described.
More recently, researchers have explored
a range of molecular cellular defects that are involved in the
development of endometriosis. The evidence for an immunological basis
to the disease continues to be explored, and some environmental toxins,
notably dioxin, have been implicated - either through a direct effect
upon steroid hormones or their receptors, or an indirect effect upon
immune system function. Peritoneal responsiveness has not been greatly
studied, but may be contributory to this disease. Without much doubt,
there is a genetic basis to endometriosis, and many researchers around
the world are attempting to identify the genetic aberrations
responsible for this disease. Allow me to return to this concept
towards the end of this dissertation, as I do believe that this will
prove to be the common thread in unravelling the complex aetiology of
endometriosis.
The cause of deep recto-vaginal
endometriosis is a subject of particular debate. In 1908, Cullen
proposed that recto-vaginal disease occurred as a result of direct
extension of lower uterine adenomyosis into the rectovaginal septum.
While this may occasionally be true, it is unlikely to explain most
cases of a common disease. Incredibly, in 1899, Russel talked about
"embryonic cell rest activation" which I interpret to be the same as
the current theory of "mullerian duct remnant metaplasia". Nissole and
Donnez2 believe that embryonic remnants in the recto-vaginal septum
undergo metaplastic change to "endometrial-like" tissue, and by
proliferation become surrounded by hyperplastic smooth muscle,
representing a typical "adenomyotic nodule" deep in the recto-vaginal
septum. Koninckx3 supports this view with evidence of altered oestrogen
and progesterone receptor activity in these nodules compared with
typical peritoneal endometriosis.
Vercellini4 approached this debate by
measuring the Pouch of Douglas (POD) depth and volume of women with and
without recto-vaginal endometriosis. He found that women with deep
endometriosis had POD depth measurements on average 1/3 less than those
without deep disease, and therefore believed that this was a primary
peritoneal disease, extending into a pseudo-recto-vaginal septum caused
by adhesion formation between the anterior rectal wall and anterior POD
peritoneum. My own observation is that rectal endometriosis often
arises from infiltrative utero-sacral disease, with involvement of the
lateral rectal wall. It seems equally likely that peritoneal POD
disease causes the majority of anterior rectal disease with
rearrangement of POD anatomy by adhesion formation. Whatever the cause,
the principles of management remain the same.
These principles depend upon an
understanding of the pathophysiology of progressive endometriosis.
Early peritoneal endometriosis must establish its own blood supply, and
in fact the pelvic distribution of endometriotic disease may have some
dependence upon the ability of disease to induce angiogenesis. Once
established, in a proportion of patients, disease is progressive.
Growth cycles induce recurrent inflammatory response and ultimately
fibrosis. Some forms of disease are marked by extreme fibrotic response
so that a fibrotic capsule comes to enclose implants. Even surface
peritoneal disease often involves much thicker fibrotic peritoneum than
first assessment would suggest. Inflamed peritoneal surfaces lead to
adhesion formation in some patients. Peri-ovarian adhesions,
colo-rectal adhesions and adhesions between pelvic organs, omentum and
small bowel predominate. Surprisingly, direct tubal involvement is
relatively uncommon.
The clinical presentation of classical
endometriosis is well known to gynaecologists. Dysmenorrhoea, pelvic
pain at other times of the cycle, abnormal uterine bleeding and
particularly premenstrual spotting, and deep dyspareunia are common
symptoms. Alternatively about 30 - 40% of patients with endometriosis
may present with infertility - and sometimes these patients are
otherwise relatively asymptomatic.
About 10% of patients with endometriosis
will have intestinal involvement. They present symptoms of deep rectal
pain, often worsened with bowel movements or exacerbated at the time of
menstruation. Disturbance of bowel habit manifesting as alternating
diarrhoea and constipation is common, and with more advanced disease
tenesmus or a feeling of incomplete rectal emptying may occur. Rectal
bleeding may be noticed, and while commonly occurring at the time of
menstruation, this is not always the case. Mucosal involvement with
endometriosis is rare. I believe that most bleeding results from trauma
to the rectal mucosa overlying endometriotic deposits, or from venous
congestion in association with an endometriotic nodule.
Patients with symptoms consistent with
inflammatory bowel disease or with rectal bleeding should undergo
colonoscopy. Very rarely will endometriosis be diagnosed at
colonoscopy. Rather, this is to exclude alternative diagnoses, or to
identify those patients with annular luminal constriction secondary to
endometriotic fibrosis.
Diagnosis may only be made by
laparoscopy. Even then deep rectovaginal endometriosis may easily be
missed when the cul de sac is obliterated. One needs to introduce an
instrument into the posterior vaginal fornix when its outline should be
clearly visible. A sponge holder is ideal for this purpose and the
isolated cul de sac obliteration will become apparent. Deep fibrotic
nodules will also be palpable on vaginal or combined rectal / vaginal
examination. Furthermore palpation of the utero-sacral ligaments with a
laparoscopic instrument will sometimes allow nodules arising from deep
within these structures to become apparent. Assessment of rectal
tethering can be enhanced by the introduction of a rectal probe or
sponge forceps into the lumen of the bowel. The extent of muscularis
involvement of serosal sigmoid deposits can also be assessed with the
aid of a probe, as the muscular layers of the bowel wall will be seen
to move independently of deposits limited to the serosa.
Treatment approaches to advanced
endometriosis in recent times have been most illogical. No amount of
progestogen and no degree of oestrogen suppression will permanently
eradicate the endometrium, so how could we expect such hormonal
approaches to eradicate endometriosis. Temporary suppression is the
only outcome, and while symptomatic improvement may occur, recurrence
of symptoms following cessation of treatment is almost invariable. No
effect on the associated fibrosis occurs, and I know of no drug of any
class that will eradicate scar. This probably accounts for the fact
that a percentage of women with deep fibrotic endometriosis fail to
experience even temporary symptom relief with hormonal suppressive
therapies.
The development of operative laparoscopy
saw many gynaecologists turn to surface ablation of peritoneal disease.
Many modalities have been used, including laser energy delivered to
peritoneal surfaces, or electrosurgical energy delivered by direct
electrode application or via Argon or Helium beams. While this may
effectively eradicate the earliest of surface disease, any deeper
disease will be inadequately treated. Furthermore it is not possible to
assess the depth of disease merely by surface visualization. Some
delivery systems are marketed on the basis of their limited depth of
penetration, and hence their safety regarding underlying critical
structures. This is inconsistent with eradication of a disease that is
invasive in all but the earliest of cases.
Back to top of page
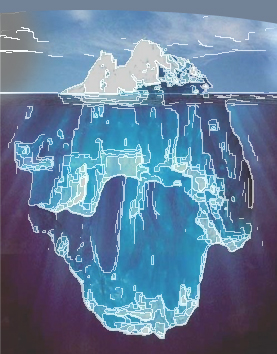
In order to avoid treating just the "tip of the iceberg", the only
logical approach must surely be surgical removal or excision of
disease. Disease overlying the ureter dictates that the ureter be
dissected free and retracted from the surgical site. Disease overlying
or involving the bowel dictates that this organ be mobilized, and
dissected free from the disease. Herein lies a problem. Certainly in my
country, the surgical training of most Gynaecologists has not equipped
them for such dissections. So patients continue to be treated with
surface ablation for deep disease, avoiding the danger sites, with
resulting treatment haphazard at best. Even worse they are subjected to
multiple courses of hormonal therapies that are known to be
ineffective, interspersed with multiple laparoscopies to "see how there
disease is going". These are about the only patients who do not need a
laparoscopy to diagnose endometriosis.
n desperation, hysterectomy and bilateral
oophorectomy is often recommended to relatively young women with
advanced endometriosis. This is often performed leaving deep disease
remaining. Not surprisingly such women often remain symptomatic.
The requirement for hysterectomy should
be determined by the presence of uterine disease. Coexistent
adenomyosis, uterine fibroids or extensive serosal involvement with
endometriosis may make hysterectomy advisable, but removal of the
normal uterus is to be avoided. Similarly, ovarian involvement with
endometriosis and its extent should dictate the need for oophorectomy.
I now wish to discuss the surgical
principles involved in the conservative excision of deep endometriosis.
This is almost always possible to achieve as a laparoscopic procedure,
with the advantages of faster patient recovery, less post-operative
adhesion formation, and most importantly improved identification and
access to deep disease. The disadvantage of course is the more
prolonged operating time. Furthermore there is no doubt that this is
complex and difficult surgery, and certainly not without risk of
serious operative morbidity.
Let us assume a patient with pelvic
sidewall disease, invasive uterosacral disease and a deep rectovaginal
nodule with bowel tethered centrally to the posterior cervix. There is
no ovarian involvement.
The patient has been thoroughly
bowel-prepped preoperatively, insufflation to 12mm Hg has been
established and an intra-umbilical 5mm endoscope has been introduced.
Three further 5mm ports have been placed, one in each iliac fossa, and
one suprapubically in the mid-line. I have two laparoscopic grhtmling
forceps (one toothed), a pair of laparoscopic scissors through which
unipolar current can be delivered, a suction irrigation probe with an
irrigation pressure generator connected via wide bore tubing and a
bipolar coagulating forceps. We also have available, if required, a 5mm
clip applicator and laparoscopic needle holders.
The first principle is to commence
dissection in an area of normality. The second principle is to use
constant tissue traction during dissection and the third is to use a
combination of high power density cut (unmodulated) current and sharp
scissor dissection. For this reason I prefer to deliver electrosurgical
current through the laparoscopic scissors. The electrosurgical
generator is set at 100W pure unmodulated current and coagulation
effect can be achieved by varying power density by altering the amount
of electrode in contact with the tissue. The bipolar output is set to
35W, and similarly delivers unmodulated current automatically.
The ureter is identified through the
peritoneum high on the pelvic sidewall and the peritoneum opened
linearly above it. The ureter can then be swept off the peritoneum in
an area where it is healthy and non-adherent. The peritoneum is then
retracted medially while dissection around all areas of disease occurs
with about a 0.5cm margin. Particular care need be taken where
overlying peritoneum is adherent to the ureter, but it is virtually
always possible to shave the ureter free from overlying disease. The
peritoneum is always found to be thicker and more fibrotic than
expected, reinforcing my belief that excision of disease is the only
logical approach. As one proceeds towards the side of the uterus,
vascular injury becomes of increasing concern. The uterine artery will
usually become apparent in its tortuous course over the top of the
ureter, and the uterine veins lateral to the insertion of the
utero-sacral ligaments become particularly prone to injury. The ureter
at this point lies more laterally and is less susceptible to injury.
Next the para-rectal spaces most be
opened. An uninvolved area of recto-sigmoid is chosen, and the
peritoneum opened on the medial side of the utero-sacral ligament. This
space may be safely opened quite deeply although bleeding from
para-rectal vessels will always be encountered. This bleeding can be
controlled with the application of electrosurgical energy through
bipolar forceps. Bleeding from the rectal sidewall can also be
controlled with bipolar energy although it is frequently prudent to use
"liga-clips" to minimise inadvertent thermal injury to the rectal wall.
Once the rectum has been mobilised
laterally, the most difficult part of the surgery commences. It is
necessary to mobilise the rectum from the posterior cervix until the
areolar tissue of the normal recto-vaginal septum is reached. It may be
possible to find a tissue plane between the nodule and the posterior
cervix / vagina, and it may be possible to find a plane between the
nodule and the rectum. More commonly the dissection proceeds through
the nodule, leaving disease both on the posterior cervix / vagina, and
on the anterior rectal wall.
With these spaces opened, it is now
possible to excise uterosacral disease to whatever depth necessary to
achieve eradication. Much reliance is placed upon trans-laparoscopic
palpation of tissues to confirm that all uterosacral disease has been
removed.
Residual rectal disease must now be
removed. It is usually possible to shave such disease from the anterior
rectal wall, but in cases of deep muscularis involvement a disc
excision may be required. Occasionally, with the greatest of care the
rectum may be inadvertently opened. Only when there is rectal stricture
formation from fibrosis, or extensive endometriotic disease involving
more than 1/3 of the rectal circumference would anterior segmental
resection be considered. In this instance, complete mobilisation of the
rectum, resection of the involved segment and either trans-anal staple
anastomosis or mini-laparotomy for a hand-sewn anastomosis is
undertaken.
Regarding repair of a rectal defect, any
hole greater than 1cm should be closed in a transverse direction. This
prevents hourglass stricturing of the rectum that could lead to
significant functional disturbance.
Rectal defects may be closed by single
layer interrupted sutures or larger defects may be closed quickly with
an ENDO GIA multifire stapling device. The articulating head stapling
devices are particularly suitable for this, as they facilitate the
desired transverse closure.
Finally, any residual disease on the
posterior cervix / vagina must be removed. This may be shaved
laparoscopically, or with deeply invasive disease may be more
efficiently removed via a vaginal approach. Excision of a segment of
vaginal wall may be required with primary vaginal closure.
If a defect in the bowel wall has been
repaired, I would leave a Penrose drain from the site of repair,
exiting through one of the lower lateral port sites. This should be
left for 5-7 days.
Before removing the ports, the pelvic and
peritoneal cavity should be copiously irrigated with saline and
haemostasis checked. It is wise to finally check haemostasis after
deflation of the pneumoperitoneum for a period of time. The
pneumoperitoneum pressure may otherwise tamponade venous bleeding sites
that only become apparent after release of this pressure.
This outlines the approach to excision of
advanced endometriotic disease. This is often long and complex surgery,
but symptomatic response to this surgery is most rewarding. Redwine and
Perez5 have reported a series of more than 500 cases of excisional
surgery for advanced endometriosis. These patients have been followed
for up to four years with significant and sustained improvement in
symptoms.
The great challenge for the future lies
in the prevention of new disease or the prevention of recurrence in
treated disease. I predict that this will occur either by genetic
manipulation or immune system modification. There is little doubt that
endometriosis has a polygenic basis, with various genetic aberrations
driving various metabolic or immunologic abnormalities. While such
research proceeds, it is less likely that these approaches will offer
hope for established, advanced fibrotic disease. Primary surgical
approaches for this problem will continue to have a place for a long
time in the future. Reference List
- Shroen D. Disputatio inauguralis medica de ulceribus uteri. Jena: Krebs, 1690:6-17
- Nisolle
M, Donnez J. Peritoneal endometriosis, ovarian endometriosis, and
adenomyotic nodules in the rectovaginal septum are three different
entities. Fertil Steril, 1997; 68:585-596
- Koninckx PR
- Vercellini
P, Aimi MD et al. Deep endometriosis conundrum: evidence in favour of a
peritoneal origin Fertil Steril, 2000; 73:1043-1046
- Redwine
DB, Perez JJ. Pelvic pain syndrome: endometriosis and midline
dysmenorrhoea. In: Arregui ME, Fitzgibbons RJ, Katkhouda N, McKernan
JB, Reich H, editors. Principles of Laparoscopic Surgery ? Basic and
Advanced Techniques. New York: Springer Verlag, 1995:545-558.
Back to top of page
|